Liver Diseases
Your liver is an important organ that performs hundreds of tasks related to metabolism, energy storage, and detoxification of waste. It helps you digest food, convert it to energy, and store the energy until you need it. It also helps filter toxic substances out of your bloodstream.
Liver disease is a general term that refers to any condition affecting your liver. These conditions may develop for different reasons, but they can all damage your liver and impact its function.
WHAT ARE THE GENERAL SYMPTOMS?
Liver disease symptoms vary, depending on the underlying cause. However, there are some general symptoms that may indicate some kind of liver disease.
These include:
- yellow skin and eyes, known as jaundice
- dark urine
- pale, bloody, or black stool
- swollen ankles, legs, or abdomen
- nausea
- vomiting
- decreased appetite
- ongoing fatigue
- itchy skin
- easy bruising
WHAT ARE SOME COMMON LIVER PROBLEMS?
Many conditions can affect your liver. Here’s a look at some of the main ones.
Hepatitis
Hepatitis is a viral infection of your liver. It causes inflammation and liver damage, making it difficult for your liver to function as it should.
All types of hepatitis are contagious, but you can reduce your risk by getting vaccinated for types A and B or taking other preventive steps, including practicing safe sex and not sharing needles.
There are five types of hepatitis:
Hepatitis A is typically spread through contact with contaminated food or water. Symptoms may clear up without treatment, but recovery can take a few weeks.
Hepatitis B can be acute (short-term) or chronic (long-term). It’s spread through bodily fluids, such as blood and semen. While hepatitis B is treatable, there’s no cure for it. Early treatment is key to avoiding complications, so it’s best to get regular screenings if you’re at risk.
Hepatitis C can also be acute or chronic. It’s often spread through contact with blood from someone with hepatitis C. While it often doesn’t cause symptoms in its early stages, it can lead to permanent liver damage in its later stages.
Hepatitis D is a serious form of hepatitis that only develops in people with hepatitis B — it can’t be contracted on its own. It can also be either acute or chronic.
Hepatitis E is usually caused by drinking contaminated water. Generally, it clears up on its own within a few weeks without any lasting complications.

FATTY LIVER DISEASE
Fat buildup in the liver can lead to fatty liver disease.
There are two types of fatty liver disease:
- alcoholic fatty liver disease, which is caused by heavy alcohol consumption
- nonalcoholic fatty liver disease, which is caused by other factors experts are still trying to understand
Left unmanaged, both types of fatty liver disease can cause liver damage, leading to cirrhosis and liver failure. Diet and other lifestyle changes can often improve symptoms and reduce your risk of complications.
Autoimmune conditions
Autoimmune conditions involve your immune system mistakenly attacking healthy cells in your body.
Several autoimmune conditions involve your immune system attacking cells and your liver, including:
Autoimmune hepatitis. This condition causes your immune system to attack your liver, resulting in inflammation. Left untreated, it can lead to cirrhosis and liver failure.
Primary biliary cirrhosis (PBC). This results from damage to the bile ducts in your liver, causing a buildup of bile. PBC can lead to eventual cirrhosis and liver failure.
Primary sclerosing cholangitis. This inflammatory condition causes gradual damage to your bile ducts. They eventually become blocked, causing bile to build up in your liver. This can lead to cirrhosis or liver failure.
Genetic conditions
Several genetic conditions, which you inherit from one of your parents, can also affect your liver:
Hemochromatosis causes your body to store more iron than it needs. This iron remains in your organs, including your liver. This can lead to damage over a long period of time if not managed.
Wilson’s disease causes your liver to absorb copper instead of releasing it into your bile ducts. Eventually, your liver may become too damaged to store more copper, allowing it to travel through your bloodstream and damage other parts of your body, including your brain.
Alpha-1 antitrypsin (AT) deficiency occurs when your liver can’t make enough alpha-1 antitrypsin, a protein that helps prevent enzyme breakdowns throughout your body. This condition can cause lung disease as well as liver disease. There’s no cure, but treatment can help.
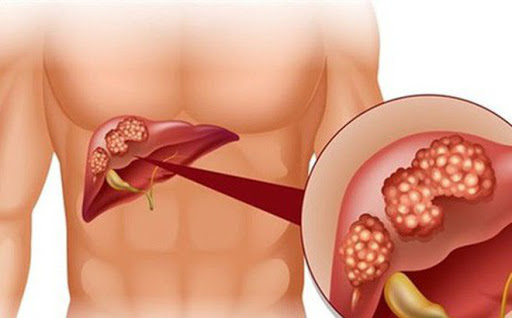
Cancer
Liver cancers first develop in your liver. If cancer starts elsewhere in the body but spreads to the liver, it’s called secondary liver cancer.
The most common type of liver cancer is hepatocellular carcinoma. It tends to develop as several small sports of cancer in your liver, though it can also start as a single tumor.
Complications of other liver diseases, especially those that aren’t treated, may contribute to the development of liver cancer.
Cirrhosis
Cirrhosis refers to scarring that results from liver diseases and other causes of liver damage, such as alcohol use disorder. Cystic fibrosis and syphilis may also lead to liver damage and, eventually, cirrhosis.
Your liver can regenerate in response to damage, but this process usually results in the development of scar tissue. The more scar tissue that develops, the harder it is for your liver to function properly.
In its early stages, cirrhosis is often treatable by addressing the underlying cause. But left unmanaged, it can lead to other complications and become life-threatening.
Liver failure
Chronic liver failure typically happens when a significant part of your liver is damaged and can’t function properly. Generally, liver failure related to liver disease and cirrhosis happens slowly. You may not have any symptoms at first. But over time, you might start to notice:
- jaundice
- diarrhea
- confusion
- fatigue and weakness
- nausea
It’s a serious condition that requires ongoing management. Acute liver failure, on the other hand, happens suddenly, often in response to an overdose or poisoning.
AM I AT RISK ?
Certain things can make you more likely to develop certain liver diseases. One of the most well-known ones is heavy drinking, which the Centers for Disease Control and PreventionTrusted Source defines as more than eight alcoholic drinks a week for women and more than 15 drinks a week for men.
Other risk factors include:
- sharing needles
- getting a tattoo or body piercing with non-sterile needles
- having a job where you’re exposed to blood and other bodily fluids
- having sex without using protection against sexually transmitted infections
- having diabetes or high cholesterol
- having family history of liver disease
- being overweight
- exposure to toxins or pesticides
- taking certain supplements or herbs, especially in large amounts
- mixing certain medications with alcohol or taking more than the recommended dose of certain medications
HOW ARE LIVER DISEASES DIAGNOSED?
If you’re concerned you might have a liver disease, it’s best to make an appointment with your healthcare provider to narrow down what’s causing your symptoms.
They’ll start by looking over your medical history and asking about any family history of liver problems. Next, they’ll likely ask you some questions about your symptoms, including when they started and whether certain things make them better or worse.
Depending on your symptoms, you’ll likely be asked about your drinking and eating habits. Make sure to also tell them about any prescription or over-the-counter medications you take, including vitamins and supplements.
Once they’ve collected all this information, they may recommend:
- liver function tests
- a complete blood count test
- CT scans, MRIs, or ultrasounds to check for liver damage or tumors
- a liver biopsy, which involves removing a small sample of your liver and examining it for signs of damage or disease
HOW ARE THEY TREATED?
Many liver diseases are chronic, meaning they last for years and may never go away. But even chronic liver diseases can usually be managed.
For some people, lifestyle changes are enough to keep symptoms as bay. These might include:
- limiting alcohol
- maintaining a healthy weight
- drinking more water
- adopting a liver-friendly diet that includes plenty of fiber while reducing fat, sugar, and salt
Depending on the specific liver condition you have, your healthcare provider may recommend other dietary changes. For example, people living with Wilson’s disease should limit foods containing copper, including shellfish, mushrooms, and nuts.
Depending on the condition affecting your liver, you may also need medical treatment, such as:
- antiviral drugs to treat hepatitis
- steroids to reduce liver inflammation
- blood pressure medication
- antibiotics
- medications to target specific symptoms, such as itchy skin
- vitamins and supplements to boost liver health
In some cases, you may need surgery to remove all or part of your liver. Generally, a liver transplant is only done when other options have failed.
Medically reviewed by Saurabh Sethi, M.D., MPH
Written by Crystal Raypole on March 21, 2019
What’s the outlook?
Many liver diseases are manageable if you catch them early. Left untreated, however, they can cause permanent damage. If you have any symptoms of a liver problem or are at risk of developing one, make sure to check in with your healthcare provider for routine checkups and testing, if needed.
https://www.healthline.com/health/liver-diseases#symptoms
Alcohol and public health: Frequently asked questions. (2018).
cdc.gov/alcohol/faqs.htm
Alpha-1 antitrypsin deficiency. (n.d.).
liverfoundation.org/for-patients/about-the-liver/diseases-of-the-liver/alpha-1-antitrypsin-deficiency
Autoimmune hepatitis. (n.d.).
liverfoundation.org/for-patients/about-the-liver/diseases-of-the-liver/autoimmune-hepatitis
Chronic liver disease and cirrhosis. (2016).
cdc.gov/nchs/fastats/liver-disease.htm
Cirrhosis. (2018).
niddk.nih.gov/health-information/liver-disease/cirrhosis/all-content
Diagnosing hepatitis C. (n.d.).
liverfoundation.org/for-patients/about-the-liver/diseases-of-the-liver/hepatitis-c/diagnosing-hepatitis-c
Hemochromatosis. (n.d.).
liverfoundation.org/for-patients/about-the-liver/diseases-of-the-liver/hemochromatosis
Liberal R, et al. (2016). Cirrhosis and autoimmune liver disease: Current understanding. DOI:
4254/wjh.v8.i28.1157
Liver cancer. (n.d.).
cancer.org/cancer/liver-cancer.html
Liver disease diets. (n.d.).
liverfoundation.org/for-patients/about-the-liver/health-wellness/nutrition
McCullough A, et al. (2017). Fatty liver disease: Get the facts.
my.clevelandclinic.org/health/transcripts/4909_fatty-liver-disease-get-the-facts
Primary biliary cholangitis. (n.d.).
niddk.nih.gov/health-information/liver-disease/primary-biliary-cholangitis
Primary sclerosing cholangitis. (n.d.).
liverfoundation.org/for-patients/about-the-liver/diseases-of-the-liver/primary-sclerosing-cholangitis
Rizza S. (2013). The ABC’s of hepatitis: Mayo Clinic expert explains types, prevention [Press release].
newsnetwork.mayoclinic.org/discussion/the-abcs-of-hepatitis-mayo-clinic-expert-explains-types-prevention
Wilson disease. (2014).
ghr.nlm.nih.gov/condition/wilson-disease

